New insights into Multiple Sclerosis treatments
 Wednesday, May 11, 2016 at 3:40PM
Wednesday, May 11, 2016 at 3:40PM Multiple Sclerosis is the most common neurodegenerative disease of young adults, affecting 2.3 million people. MS is insidious. It can lie dormant for years, controlled well by treatment, but there is no cure and patients always live with the threat of another attack that takes away more of their function. One of the frustrating aspects of MS is that we have treatments, but we don't really understand them. There are plenty of drugs that work to control MS, but it is impossible to predict which drug will work well for which patient, or how long that drug will work. We don't even really understand the way that the different drugs function - essentially, it is a guessing game to find which treatment will work best in which patient; a guessing game that dangerously chews up time as the disease progresses.
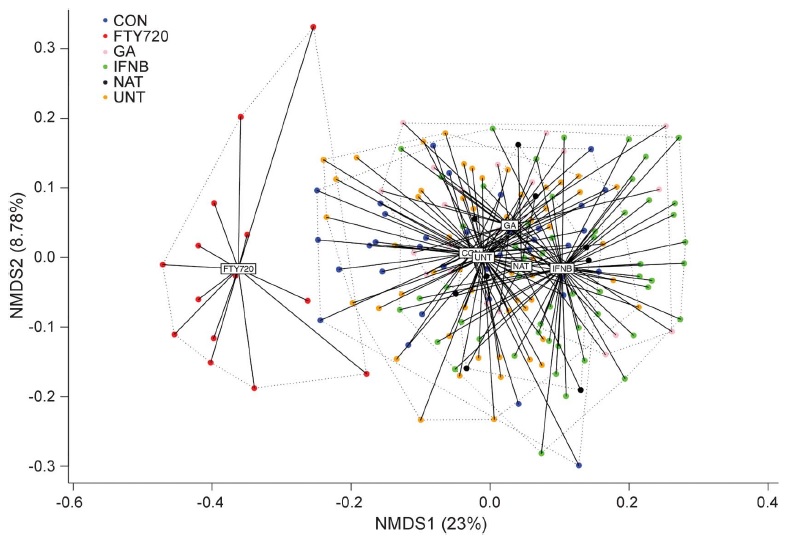
In a major new study just released, the Translational Immunology laboratory teamed up with the Neuroimmunology laboratory (led by Prof An Goris) and performed the first large-scale in-depth immunological analysis of multiple MS treatments. We profiled the immune systems of 245 individuals, including untreated MS patients and MS patients being treated with four standard treatments - interferon-beta, glatiramer acetate, natalizumab, or fingolimod. Since all the treatments are effective in at least some patients, we had expected to find that each treatment ould have a similar impact on the immune system. Instead, the results were surprising - each of the treatments did something different to the immune system.
In fact, the only common response we found to MS treatment was an increase in the serum cytokine BAFF. The confusing part is that BAFF was thought to be detrimental during MS - several mouse trials found that increased BAFF drives more severe disease, while inhibiting BAFF cured disease. These mouse results were strong enough that two clinical trials had started injecting anti-BAFF antibodies into MS patients in the hope of stopping disease progress. And yet, we found that BAFF was going up in patients that were given multiple different effective MS treatments! Our model suggests that increased BAFF may actually be a protective part of MS treatment, so is it wise to give MS patients anti-BAFF? Unfortunately, our model appears to be correct, as the two trials of BAFF in MS have now been prematurally stopped, due to excessive adverse events.
There are three major lessons to be learned from our study:
First, we should look at testing drugs that increase BAFF rather than decreasing BAFF. This may be a promising avenue for treating MS in patients that do not respond to existing drugs.
Second, we should stop assuming that we understand how existing drugs work. Every drug that we give has multiple impacts on the body, and we should not assume that we know which of these impacts are the protective ones. By identifying which particular impacts are shared across multiple effective drugs, then we are more likely to be looking at the protective effects. If our study had been performed earlier, then I doubt anyone would have gone ahead and given anti-BAFF antibodies to MS patients, and these adverse events could have been avoided.
Third, further large-scale immune analyses such as ours may allow us to predict which patients will respond to which drugs best. In MS this is critical - time spent on an ineffective drug means function is lost that will not be regained - patients need the right drug as soon as possible.
You can read more about our study at Neurology: Neuroimmunology & Neuroinflammation:
Dooley*, Pauwels*, Franckaert, Smets, Garcia-Perez, Hilven, Danso-Abeam, Terbeek, Nguyen, De Muynck, Decallonne, Dubois, Liston* and Goris*. 'Immunologic profiles of multiple sclerosis treatments reveal shared early B cell alterations'. 2016 vol. 3 no. 4 e240
 Liston lab,
Liston lab,  Medicine,
Medicine,  immunology,
immunology,  neuroscience
neuroscience 

Reader Comments (1)
Thank you for your article. I found this useful.
Advanced Skin Lounge, Acne treatments Leeds
http://www.advancedskinlounge.co.uk