Dieet met veel suiker verhoogt risico op pancreaskanker
 Tuesday, July 28, 2020 at 7:22PM
Tuesday, July 28, 2020 at 7:22PM
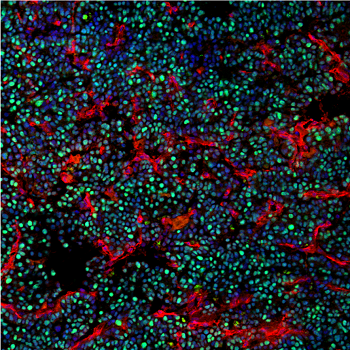
Suikerrijke voeding veroorzaakt de ontwikkeling van alvleesklierkanker en verhoogt de kans op een dodelijke afloop. Tot die bevinding zijn onderzoekers van het Vlaams Instituut voor Biotechnologie (VIB) en de KU Leuven gekomen.
Een suikerrijk dieet verhoogt niet alleen de kans op het ontwikkelen van pancreaskanker. Het stimuleert ook de agressieve groei van tumoren. Tot die conclusie komen onderzoekers van VIB-KU Leuven en collega's van het Babraham Institute van de Britse universiteit Cambridge.
De resultaten zijn gepubliceerd in het tijdschrift Cell Reports.
Alvleesklierkanker is een zeldzame maar dodelijke vorm van kanker door late detectie en een slecht begrip van risicofactoren. Bekende risicofactoren zijn obesitas, voeding en diabetes type 2, maar door de lage incidentie en de onderlinge samenhang is hun individuele bijdrage moeilijk in te schatten.
De onderzoekers voltooiden een uitgebreid project met experimenteel werk bij muizen en menselijke gegevens. Bij de dieren werd de progressie van pancreaskanker beïnvloed door voedingssuiker, met een snellere tumorgroei en verhoogde dodelijkheid.
Het effect bij mensen blijkt hetzelfde. Bij 500 deelnemers aan de studie onderzochten de onderzoekers de interactie tussen genen en voeding en ontdekten dat hoge niveaus van voedingssuiker het risico op alvleesklierkanker verhoogden. 'We hebben jarenlang gekeken naar verschillende voedings- en genetische veranderingen en niets komt in de buurt van de nadelige gevolgen van een dieet met veel suiker', zegt James Dooley, senior wetenschapper bij het Babraham Institute.
Plantaardige voeding met een equivalent van een avocado per dag vermindert het risico op pancreaskanker met tien procent.
 Liston lab,
Liston lab,  cancer,
cancer,  metabolism
metabolism