As people age, they often experience problems with their memory and cognitive abilities. This happens in part because their brains become mildly inflamed. But there may be a solution: a small group of special T cells, called regulatory T cells, could help reduce this inflammation in aging brains. Administering a protein called interleukin-2 (IL2) can help these special T cells grow and prevent inflammation. Now, researchers at VIB, KU Leuven, Babraham Institute, and i3S have tested this approach in mice and found that it can prevent neurological decline. Their findings, published in EMBO Molecular Medicine suggest that targeting the immune system might keep people’s brains healthy as they age.
Emanuela Pasciuto, co-first author of the study: “Our goal was to see whether we could slow down the aging process of the brain by changing its immune system through the delivery of IL2. We know that inflammation plays a significant role in various aging processes, and IL2 could help us tilt the balance back in our favor.”
Inflammation in the aging brain
 Aging is a degenerative process that affects the whole body, including the brain. As we age, our brains may experience cognitive decline, affecting our memory and ability to think clearly. Increasing evidence suggests that inflammation in the brain, called “inflammaging,” can worsen this decline. Inflammaging is caused by immune cells entering the brain as we age. This inflammation can activate microglia, the resident immune cells in the brain, and induce neuroinflammation, leading to cognitive decline and dementia.
Aging is a degenerative process that affects the whole body, including the brain. As we age, our brains may experience cognitive decline, affecting our memory and ability to think clearly. Increasing evidence suggests that inflammation in the brain, called “inflammaging,” can worsen this decline. Inflammaging is caused by immune cells entering the brain as we age. This inflammation can activate microglia, the resident immune cells in the brain, and induce neuroinflammation, leading to cognitive decline and dementia.
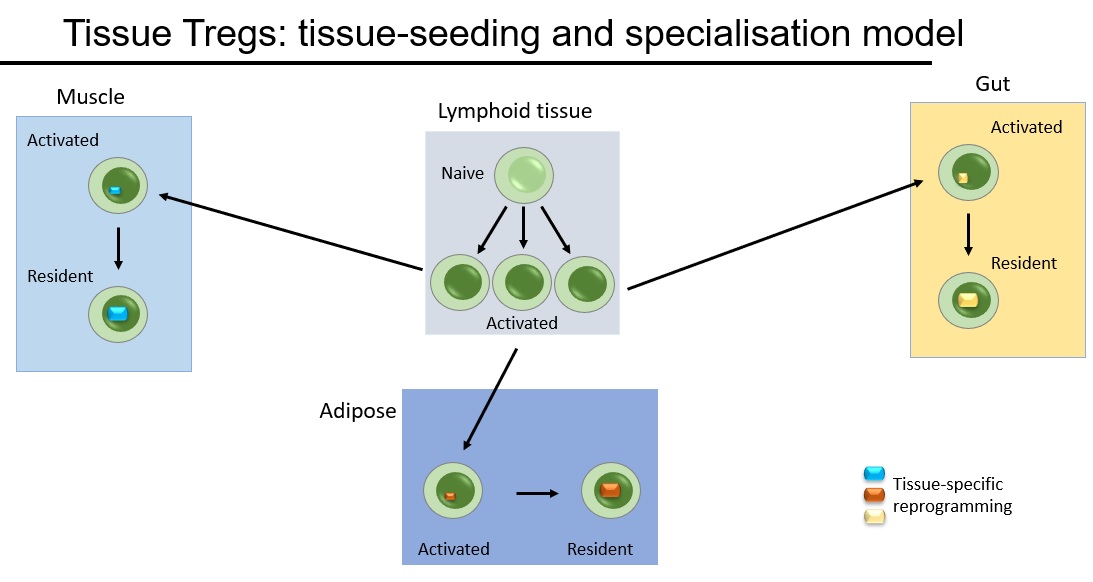
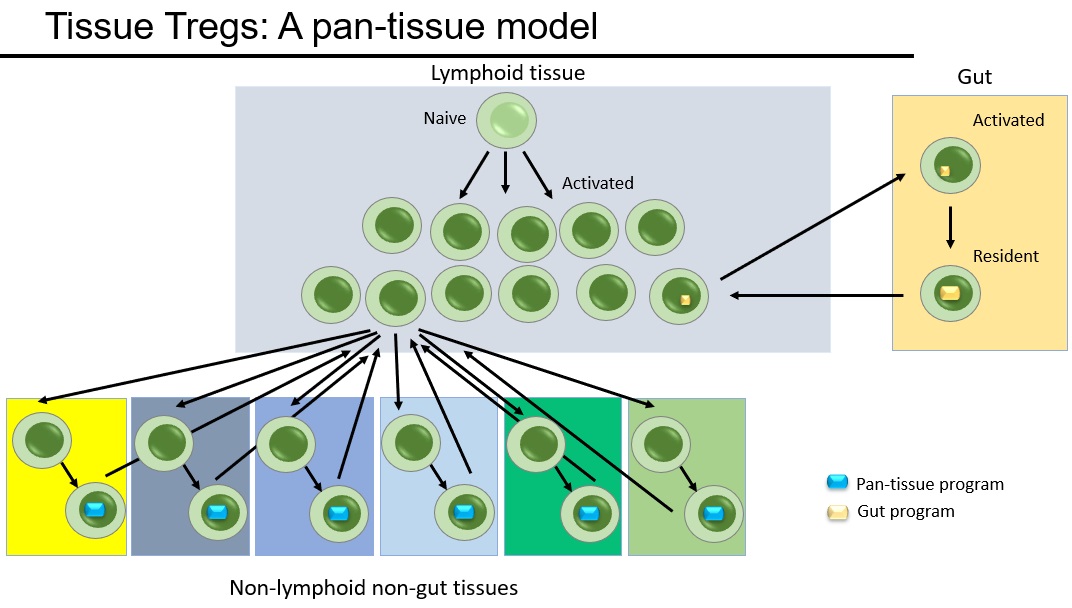
However, researchers have found a way to reduce inflammation in the brain by targeting a small group of special immune cells in the brain called regulatory T cells. Previously, the team of Adrian Liston (VIB-KU Leuven, Babraham Institute) and Matthew Holt (VIB-KU Leuven, i3S Porto) showed that administering a protein called Interleukin-2 (IL2), which helps regulate the immune response, increased the number of regulatory T cells in the brain. This treatment has been successful in mouse models of traumatic brain injury and neuroinflammation.
Now, the researchers want to see if delivering IL2 directly to the brain can help reduce age-induced inflammation and cognitive decline.
Gene therapy improves brain aging
In their latest study, the team discovered that delivering IL2 to the brain improved brain function in aging mice. The research showed that the treatment restored cognitive performance in spatial memory tests, allowing older mice to form new memories almost as well as young mice. The mice given IL2 treatment were better at remembering visual cues than those that did not receive the treatment. Additionally, some of the changes in cellular aging in the brain were reversed, especially among several types of glial cells, which are critical to support overall brain function and health.
Pierre Lemaitre, co-first author of the study: “Our approach was to harness the body’s own system to regulate inflammation and to boost it precisely where it was needed.”
IL2 was delivered to the brain using a gene therapy vector, which is a tool that provides genetic material to specific cells. The additional dose of IL2 allowed the regulatory T cells to survive and create an anti-inflammatory environment. Matthew Holt and Lidia Yshii, co-senior authors of the study: “This reinforces our belief that viral vector-based systems are the way forward for the delivery of therapeutics to combat chronic neurodegenerative diseases and preventing cognitive decline in aging populations.”
Adrian Liston, senior author of the study: “The most important part of this study is the high potential for translation into patients. Inflammation is a process that is conserved in both mice and humans, and regulatory T cells can respond to IL2 in both species. However, there are still regulatory hurdles to clear, and it’s crucial to ensure safety before testing it in patients. Nonetheless, we see a clear path to conducting clinical trials.”
The laboratory is working through spin-off company Aila Biotech to drive entry of this therapeutic into clinical trials. Read the full study here.
 Sunday, April 21, 2024 at 12:37AM
Sunday, April 21, 2024 at 12:37AM  immunology
immunology