A mysterious inflammatory disease has been afflicting a Flemish family for three generations, causing severe skin lesions, fevers, pain and exhaustion. This disease, which previously had no known cause or cure, has now been identified as Pyrin Associated Autoinflammation with Neutrophilic Dermatosis (PAAND), and has also been found in families in England and France. New research by Adrian Liston (VIB/University of Leuven, Belgium), Seth Masters (Walter and Elisa Hall Institute, Australia), Carine Wouters (University of Leuven, Belgium) has found the genetic mutation causing the disease and also identified an effective treatment. This research was published in the international scientific journal Science Translational Medicine.

For decades, families in Belgium, England, and France have been living with a mysterious disease that results in skin lesions, fevers, pain and exhaustion. Every generation, half of the children of the people with this disease develop the same symptoms. Doctors had been previously unable to identify the disease or find any effective treatment. For the first time, this disease has been identified and a treatment found due to an international research team.
Professor Adrian Liston (VIB/University Leuven): “Detailed work by clinicians told us that we were dealing with a genetic disease. Thanks to advances in DNA sequencing technology we were able to sequence the genome of these patients and find the mutation causing the disease”.
The mutation is in the gene called MEFV. This gene was known to cause an inflammatory disease called Familial Mediterranean Fever (FMF) in patients who inherit mutated copies from both mother and father. However, the mutation found in the PAAND patients is different. Only a single copy of the mutation is needed to cause disease, meaning it affects half the children of patients, unlike the mutations that cause FMF, which often skip generations.
Professor Seth Masters (Walter and Elisa Hall Institute): “The PAAND mutation causes the body to as if there is a bacterial skin infection. This leads to the skin making the inflammatory protein interleukin-1β, which causes skin lesions, fevers and pain”.

A cure for the new disease?
Understanding the biological basis for this new disease allowed the rational selection of a new treatment. The researchers repurposed an anti-arthritis drug, anakinra, which targets the same protein that causes PAAND, interleukin-1β. The results in the first volunteer, from an English family, were striking, with a rapid clearance of skin lesions and a complete recovery from fevers and pain. A larger trial is now beginning in the Flemish patients to see if this targeted treatment will act as a complete cure.
Professor Carine Wouters (KU Leuven/UZ Leuven, lead clinical researcher): “This is the synthesis of an intense collaboration between clinicians and scientists trying to understand this disease for almost 10 years. I am delighted to see how it has increased our understanding of rare mutations, and especially has opened a therapeutic perspective for these patients.”
Quote from one of the patients: “We are happy and very grateful to the doctors and scientists who never gave up their search to understand the disease that affected members of our family for so many years. We are very hopeful that the new treatment will be beneficial to our family. Also we realize that the findings will help other patients to get a correct diagnosis and therapy.”
Professor Adrian Liston (VIB/KU Leuven, lead scientific researcher): “This is an amazing time to be working on genetic diseases. Every month we are solving clinical cases that would have been too hard to work out just a few years ago. Actually, to be honest the research is moving much faster than the healthcare system – we are finding new mutations, new diseases and trialling new treatments faster than the healthcare system is adapting. It creates a difficult situation for patients where the science is in, but the health insurance funds are not ready to reimburse the costs of the advanced diagnostic tests we use or novel treatments that we discover. This is a challenge, but also an opportunity – medical improvements could be rolled out quite quickly with political will.”
Professors Carine Wouters and Adrian Liston have established the charity Ped IMID to seek funding for research, diagnosis, and treatment of people living with rare immune disorders not currently covered by the health insurance funds.
To read more, go to our article in Science Translational Medicine:
Masters, Lagou, Jéru, Baker, Van Eyck, Parry, Lawless, De Nardo, Garcia-Perez, Dagley, Holley, Dooley, Moghaddas, Pasciuto, Jeandel, Sciot, Lyras, Webb, Nicholson, De Somer, van Nieuwenhove, Ruuth-Praz, Copin, Cochet, Medlej-Hashim, Megarbane, Schroder, Savic, Goris, Amselem, Wouters* and Liston*. Familial autoinflammation with neutrophilic dermatosis reveals a regulatory mechanism of pyrin activation. Science Translational Medicine. 2016 in press.
 Thursday, June 23, 2016 at 12:16PM
Thursday, June 23, 2016 at 12:16PM 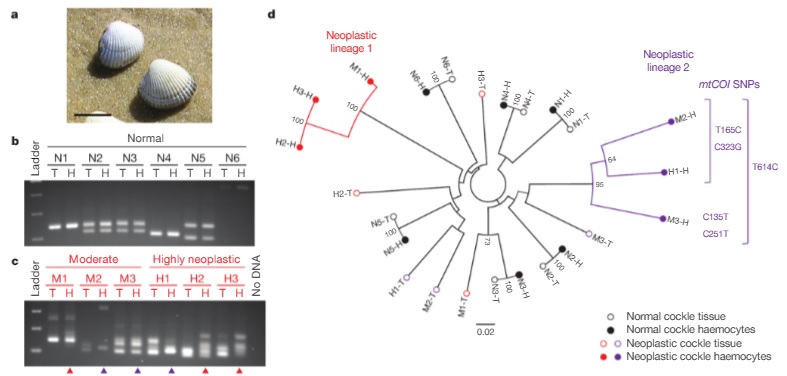
 Medicine,
Medicine,  cancer,
cancer,  immunology
immunology